How Soap Notes Paved The Way For Modern Medical
Soap Notes On The App Store
Understanding Soap Format For Clinical Rounds Global Premeds
Whether you're interested in reviewing information doctors have collected about you or you need to verify a specific component of a past treatment, it can be important to gain access to your medical records online. this guide shows you how. Offers a computer based medical record including templating, soap notes, and records soap medical patient demographics.
40 Fantastic Soap Note Examples Templates Templatelab
Chart providing details of maine medical records laws internet explorer 11 is no longer supported. we recommend using google chrome, firefox, or microsoft edge. are you a legal professional? visit our professional site » created by findlaw'. tampa natives on facebook our two scents handmade soaps tampa midwife records pictures of cuba most of t he photos Medical records privacy laws outline patients' rights to secrecy of their records soap medical medical information, and the circumstances under which that information may (or must) internet explorer 11 is no longer supported. we recommend using google chrome, f.
Soap notes are used for admission notes, medical histories and other documents in a patient’s chart. many hospitals use electronic medical records, which often have templates that plug information into a soap note format. most healthcare clinicians including nurses, physical and occupational therapists and doctors use soap notes. Best practices: problem-oriented medical record and soap notes. september 3, 2015. 0. 0. evidence in integrative healthcare. in 1968, lawrence weed, md, developed the problem-oriented medical record (pomr) “… to develop a more organized approach to the medical record…” (weed l. medical records that guide and teach. nejm vol. 278, no. 11. The add new screen allows you to enter a new listing into your personal medical events record. an official website of the united states government the. gov means it’s official. federal government websites always use a. gov or. mil domain. b. The soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare providers to write out notes in a patient's chart, along with other common formats, such as the admission note. documenting patient encounters in the medical record is an integral part of practice workflow starting with appointment scheduling, patient check-in and exam.
It’s a patient’s right to view his or her medical records, receive copies of them and obtain a summary of the care he or she received. the process for doing so is straightforward. when you use the following guidelines, you can learn how to.
Developed by dr/ lawrence weed in the 1960s, the soap note template methodology records vital patient medical information, to provide evidence of patient contact, and to inform a clinical reasoning process. soap notes have four main parts, designed to help improve evaluations and standardize documentation: subjective what the patient tells you. Soap notes is a robust patient manager app that is specifically designed to allow for quick, accurate soap notes for each patient's visit. soap notes is ideal for any person who must manage detailed notes for each patient visit and needs an app that will enter the notes quickly, and accurately. Documenting a patient assessment in the notes is something all medical students need to practice. this guide discusses the soap framework (subjective, objective, assessment, plan), which should help you structure your records soap medical documentation in a clear and consistent manner.
Shown above is an example of a medical soap note that discusses the present state of a patient who came to the clinic to seek answers for a few complaints. practitioners tend to go into detail with their analysis to gather a sufficient amount of information for their records. 6. nutrition medical soap note. The soap note was first introduced into the medical field by dr. lawrence weed in the early 1970s and was referred to as the problem-oriented medical record (pomr). at the time, there was no standardized process for medical documentation. Each time you hop up on a doctor's exam table, somebody makes a note in your medical records. there may come a time when you need your medical information, so find out how to get it and how it's protected. each time you climb up on a doctor. Documenting a patient assessment in the notes is something all medical students need to practice. this guide discusses the soap framework (subjective, objective, assessment, plan), which should help you structure your.
The soap note stands for subjective, objective, assessment, and plan. this note is widely used in medical industry. doctors and nurses use soap note to document and record the patient’s condition and status. the soap note is considered as the most effective and standard documentation used in the medical industry along with the progress note. A hacker claims to have stolen just shy of 10 million records, and is putting them on for sale on the dark web for about $820,000. the hacker posted the records on the site therealdeal, and the data includes social security numbers, address. A soap note, records soap medical or a subjective, objective, assessment, and plan note, contains information about a patient that can be passed on to other healthcare professionals. to write a soap note, start with a section that outlines the patient's symptoms and medical history, which will be the subjective portion of the note.
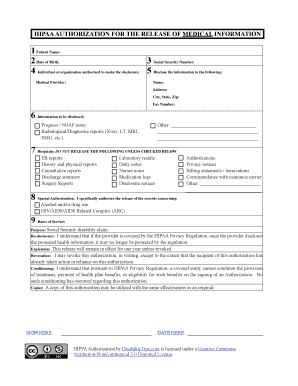
Confidential patient medical records are protected by our privacy guidelines. patients or representatives with power of attorney can authorize release of these documents. we are experiencing extremely high call volume related to covid-19 va. Soap notes are commonly found in electronic medical records (emr) and are used by providers of various backgrounds. generally, soap notes are used as a template to guide the information that physicians add to a patient's emr.
A soap note template comes in a very structured format though it is only one of the numerous formats health or medical professionals can use. a soap note template by a nurse practitioner or any other person who works with the patient enters it into the patient’s medical records in order to update them. A soap (subjective, objective, assessment, plan) note is a method of documentation used specifically by healthcare providers. soap notes are used so staff can write down critical information concerning a patient in a clear, organized, and quick way. soap notes, once written, are most commonly found records soap medical in a patient’s chart or electronic medical records.
Soap or soap notes as they are widely called also find extensive usage in veterinary practices. it is a way for clinics to record, document, and store patient’s medical information in a systematic way. it also gives the practice a framework to evaluate information without losing even the tiniest bit. The soap note format gives a full picture of your pet’s quality of care and medical history by breaking down any surgical history, diagnostic test results, physical exams, x-ray results, current medications, and objective data that will help your pet’s healthcare provider build the perfect treatment plan for whatever your pet is facing. this. Soap finds its usage in recording patient progress. soap or soap notes as they are widely called also find extensive usage in veterinary practices. it is a way for clinics to record, document, and store patient’s medical information in a systematic way. A propublica report found more than 180 servers on which people’s medical records were available with minimal or no safeguards. an award-winning team of journalists, designers, and videographers who tell brand stories through fast company's.